International Journal of Anatomical Sciences 2010, 1: 14-16
Research Paper
A Study on the incidence of Retromolar Foramen and Canal in Indian
Dried Human Mandibles and its Clinical Significance
Senthil Kumar S, Kesavi D.
Department of Anatomy, Sri Ramachandra Medical College and Research Institute
Sri Ramachandra University, Chennai 600 116, Tamil Nadu, India.
Key Words: mandible, third molar, retromolar canal & retromolar foramen
Abstract: The retromolar foramen (RMF) is one of the nonmetrical variants of the mandible (Ossenberg, 1987). The dental practitioners should be aware of this variant and the possible complications which may occur during anesthetic, surgical, and implantation procedures of the mandible .Indian adult dried human mandibles (150) were observed for the presence of retromolar foramen (RMF) or retromolar canal. Their gross morphological features were studied. These canals showed variations in location, length and diameter in relation to third molar.
Many people require removal of their third molar also known as wisdom teeth. As with any surgical procedure, there are some possible risks and complications (Anderson, 1998). The lower third molar region includes the area in which this tooth, its supporting elements and the adjacent soft parts, the lingual nerve and the elements of the paralingual space. Posterior to lower third molar there is a cribose triangular surface, the retromolar triangle and the retromolar fossa laterally (Suazo et al.,2007). The cribose area of the retromolar triangle communicates with the mandibular canal, describing it via an anesthetic technique for the inferior alveolar nerve block (Suazo et al., 2008, Sandoval et al.,2008). Clinically, this region is covered by an elevation of mucosa of variable size.
Correspondance to: Senthil Kumar S, Department of Anatomy, Sri Ramachandra Medical College and Research Institute, Sri Ramachandra University Porur, Chennai 600116, India
Email: [email protected]
Retromolar fossa is a depression where the buccinator muscle is attached above the inferior alveolar canal. From a clinical point of view this area forms, a open corridor for the passage of infections arising in connection with the third molar, this is the so-called Chompret-L’ Hirondel abscess (abcès migrateur de Chompret-L’Hirondel) used it path (Libersa et al., 1982; Peron,2004). On the surface of the retromolar fossa found the retromolar foramen (RMF), which creates a canal of variable depth, regarded as an anatomical variation. Since most of the anatomical books do not mention about this foramen or canal this study was undertaken to analyze the incidence in Indian adult dried mandibles.
Materials and Methods
A total of 150 Indian adult dried human mandibles were observed for the presence of retromolar foramen (RMF) or retromolar canal in Department of Anatomy, Sri Ramachandra Medical College and Research Institute. Their locations in relation to third molar were taken into account for observation. The diameter and the depth were measured by using Mitutoyo’s Dial Caliper.
Observations
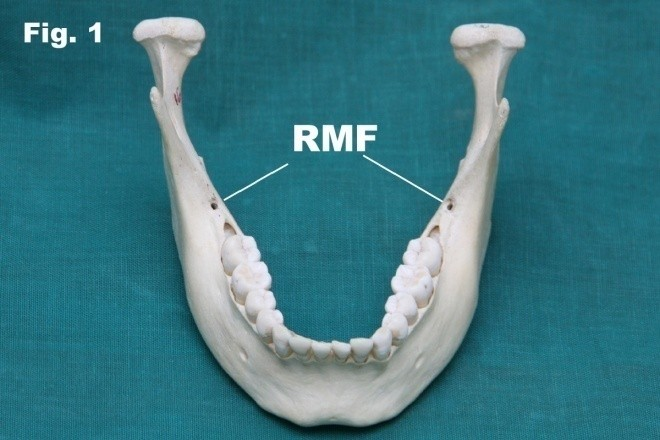
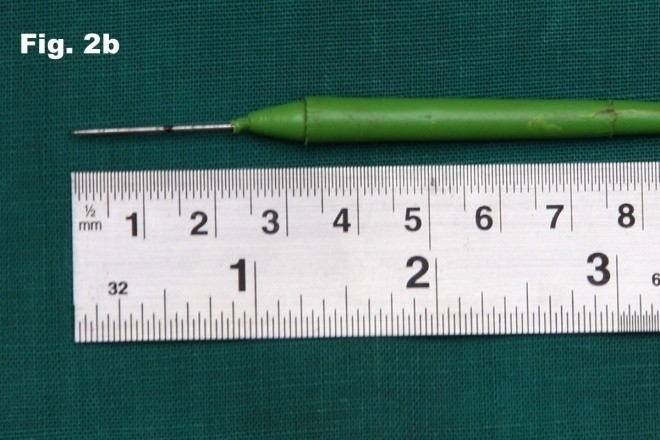
The retromolar foramen and canal Fig. 1 was found in 26 of 150 mandibles (17.3%) of which 8 on the right side (5.3%),6 on the left side (4%) and 12 bilaterally (8%) (Table I). The depth of the retromolar foramen and canal was found to be an average of 12mm Fig.2a and 2b. The diameter of the retromolar foramen and canal was found to be an average of 1.3 mm. The distance between posterior third molar to retromolar foramen and canal was found to be an average of 4.5 mm on the right side and 4mm on the left side Fig.3. The distance between anterior border of ramus to retromolar foramen was found to be an average of 8.4 mm on the right side and 8.3mm on the left side. The distance between lingula to retromolar foramen was found to be an average of 14.1mm on the right side and 12.6mm on the left side.
Table 1 Distribution of Retro Molar Foramen
|
From the above observations the occurrence of RMF was more in females compared to males. The diameter of RMF was found to be larger in the right side. The distance of RMF from third molar, anterior border of ramus and lingula are also found to be higher on the right side. The bilateral occurrence of RMF was found to be higher in females.
Fig. 1 Photograph showing retromolar sides.
|
|
Fig. 2a Photograph showing the depth of foramen on both retromolar foramen on the right side.
|
|
Fig. 2b Photograph showing the measurement retromolar canal.
|
|
Fig. 3 Photograph showing retromolar foramen of the depth of on the left side.
|
|
Discussion
The incidence of RMF located in the retromolar fossa, in our study was 17.3%. It is higher than what reported earlier by Suazo, et al., (2008) 12.9% in Brazilians, but lower than what reported by Kodera & Hashimoto, (1995) 19.5% in Japanese population and Narayana et al., (2002) 21.9% in the South Indian population.
Kodera and Hashimoto (1995) per- formed the dissection of retromolar canal in Japenese cadavers and found within the retromolar canal, the artery running was a branch from the inferior alveolar artery, it ran through the canal forwards and joined with the branches of the buccal artery and the facial artery. The nerve in the retromolar canal was a branch from the trunk of inferior alveolar nerve and branched off to the following areas: the third mandibular molar, the mucosa of retromolar triangle, the buccal mucosa, and the buccal gingiva of the mandibular premolar and molar region. These elements may be injured in the dieresis procedures, flap lifting, bone tissue for autologous bonegrafts, osteotomy for the surgical extraction of lower third molars, placement of osseointegrated implants for orthodontic or during the division of the mandibular ramus in the sagittal split osteotomy surgery (Reyneke et al., 2002 , Boronat Lopez and Peñarrocha Diago, 2006).
This study clearly establishes the incidence of the retromolar foramen and its clinical significance. The retromolar foramen is highly variable in their morphology and morphometry. The cortical plate over the retromolar triangle is not heavy as the bone surrounding it and it is more cancellous (Ash et al., 2003). During routine anesthetic, surgical and implantation procedures of the mandible, care should be taken not to damage the neurovascular bundle passing through the retromolar foramen.
References Anderson M (1998) Removal of asymptomatic third molars: indications, contraindications, risks and benefits. J Indiana Dent Assoc, 77: 41-46.
Ash M, Nelson SJ (2003) Wheelers dental anatomy, physiology and occlusion, 8th Edition, Elsevier Publishers, St Louis, MO. 398.
Boronat López A, Peñarrocha Diago M (2006) Failure of locoregional anesthesia in dental practice. Review of the literature. Med Oral Patol Oral Cir Bucal, 11: E510-513.
Kodera H, Hashimoto I (1995) A case of mandibular retromolar canal: elements of nerves and arteries in this canal. Kaibogaku Zasshi, 70: 23-30.
Libersa JC, Francke JP, Boudin G, Goudaert M, Libersa C (1982) Anatomical basis for the surgical approach to the dental roots. Anat Clin,3: 221-227.
Narayana Nayak UA, Ahmed WN, Bhat JG, Devaiah BA (2002) The retromolar foramen and canal in south Indian dry mandibles. Eur J Anat, 6: 141–146.
Ossenberg NS (1987) Retromolar foramen of the human mandible. Am J Phys Anthropol, 73, 119-128.
Peron JM (2004) Accidents d’évolution des dents desagesse. EMC – Dentisterie, 1 : 147-158.
Reyneke JP, Tsakiris P, Becker P (2002) Age as a factor in the complication rate after removal of unerupted impacted third molars at the time of mandibular sagittal split osteotomy. J Oral Maxillofac Surg, 60: 654-659.
Sandoval MC, Suazo GI, Cantín LM, López FB (2008) Pilot study of the inferior alveolar nerve block anesthesia via the retromolar triangle in patients of 40 to 60 Years. Int J Odontostomat,2: 8-13.
Suazo GI, Cantín LM, López FB, Valenzuela UV, Valenzuela RR (2007) Morphometric study of the retromolar triangle. Int J Odontostomat, 1:129-132.
Suazo I, Cantín M, Zavando D (2008) Inferior alveolar nerve block anesthesia via retromolar triangle, analternative for patients with blood discrasias. Med Oral Patol Oral Cir Bucal, 13: E43-E47.