International Journal of Anatomical Sciences 2011, 2(2): 34-36
Case Report
Cystic Duct Remnant Syndrome Associated with Symptomatic Dilatation of Cyst Duct
Arun Kumar S. Bilodi, Gangadhar MR.
Department of Anatomy, Mahatma Gandhi Medical College, Pilliyarkuppam, Puducherry. (Union territory), India.
Department of Anthropology, Manasagangothri, University of Mysore, Mysore, Karnataka, India
Abstract: A case of recurrent abdominal (biliary tract) symptoms, mimicking gallbladder disease after previous cholecystectomy is presented. The symptoms were attributable to a long residual cystic duct stump with low insertion which was missed at previous surgery. The residual stump had undergone dilatation mimicking a gallbladder. Awareness of anomalies and variations of the extra hepatic biliary tree is necessary to avoid such unforeseen complications.
Key words: residual cystic duct stump, anatomical variations, post cholecystectomy syndrome, cystic duct remnant syndrome.
Variations in cystic duct anatomy are not uncommon and reported incidences vary from 18% -23%. There may be variable length of cystic duct, variable course, and variable insertion. The cystic duct joins the common bile duct in its distal part in 9-11% (Taourel et al., 1996; Turner and Fulcher,2001; Tsitouridis et al., 2007). Failure to recognize these variations may lead to ductal ligation, biliary leaks or strictures after laparoscopic cholecystectomy (Suhocki and Meyers, 1999; Marcos, 2000). Any failure to recognize these variations may lead to ductal ligation, biliary leaks or strictures after laparoscopic cholecystectomy (Suhocki and Meyers, 1999; Marcos, 2000). Of the anomalies one of the most significant is a low insertion of the cystic duct with the long cystic duct running parallel to or behind the common bile duct. This anomaly is difficult to recognize on the table unless the surgeon is aware of this variation because ‘what your mind does not know your eyes can not see’.
Case Report
A 57 years old male, presented with history of pain in the right upper quadrant of the abdomen with nausea and occasional vomiting. There was no history of fever or obstructive jaundice. Past history revealed that he had undergone a laparoscopic cholecystectomy ten years earlier. Surgery and immediate postoperative period were uneventful. He developed recurrent abdominal pain and jaundice a year after surgery. Endoscopic retrograde cholangiopancreatography (ERCP) showed a residual Common Bile Duct (CBD) stone which was extracted after sphincterotomy. A temporary stent was inserted for two months with complete relief.
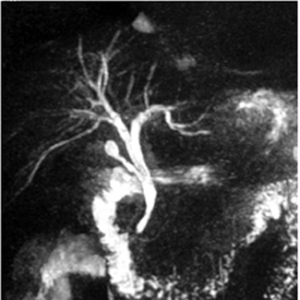
In the current presentation there were no abdominal findings. Routine hematological and urinary examinations were normal. Ultrasound showed absent gall bladder with no other positive findings. Since symptoms were suggestive of recurrent biliary disease, a Magnetic Resonance Cholangiopancreatography (MRCP) was advised. This showed a long cystic duct remnant, low insertion of the cystic duct and dilatation of the residual cystic duct mimicking a ‘neo-gall bladder’ (Cystic duct remnant syndrome). He was put on cholagogues and advised regular follow up.
Fig. 1 MRCP showing dilatation of stump of cystic duct into a fusiform dilatation –‘neo gall bladder’
Discussion
The cystic duct is subject to several anatomical developmental/congenital variations such as i) the cystic duct and common hepatic duct running parallel with a low confluence of cystic duct (Lamah et al.,2001) ii) insertion of the cystic duct in the right or left hepatic duct and bifurcation of left and right hepatic ducts (Lamah et al.,2001) iii) anterior, posterior or spiral types of insertion of the cystic duct iv) absence or short cystic duct (less than 5mm) v) double cystic duct (Fujikawa et al., 1998; Bernard et al., 2001) vi) the right hepatic duct emptying into the cystic duct (Hashimoto et al., 2002) vii) hepatico-cystic duct (Loasnoff et al., 2002).
Developmentally, it is from the pars cystica of hepatic bud arises both gall bladder and cystic duct. The bile duct arises also from hepatic bud proximal part to pars cystica. During development bile duct opens first on ventral aspect of duodenum, when rotation of duodenal loop occurs, bile duct opens on the dorsomedial aspect of duodenum (Singh and Pal, 2007). Developmental anomalies such as Sessile Gall Bladder – direct opening of gall bladder into bile duct, agenesis – absence of gall bladder and diverticulum from any part of the gall bladder has been documented (Singh and Pal, 2007).
Anatomical variations regarding the duct system have also been documented previously (Singh and Pal, 2007). This includes termination cystic duct on the left side of common hepatic duct, termination of cystic duct into right hepatic duct, opening into common hepatic duct after passing anterior to the duodenum, opening of bile duct into either pyloric part or cardiac part or at end of stomach, partial or complete atresia of duct system, duplication of parts of duct system etc. Knowledge about the possible anatomical variations is of importance for successful treatment.
Various authors have studied and reported on complications due to cystic duct variations. The left out cystic duct stump have frequently caused complications of cholecystectomy. Rogy et al., (1991) has reported post operative complication following cholecystectomy in 10% which was due to remnant of cystic duct. Walsh et al., (2002) has reported that remnant of cystic was the cause of relapse or recurrence of symptoms after cholecystectomy. It is preventable by identifying junction of cystic duct with CBD per operatively (Walsh et al.,2002). Tantia et al., (2008) also has reported left out cystic duct causes problems. Wani et al., (2010) has labeled this condition as post cholecystectomy Mirrizzi Syndrome.
MRCP and ERCP remain the definitive methods of assessing cystic duct anatomy. Of the two, MRCP is less invasive. Shaw et al., (2004) has considered that MRCP is the best method of diagnosis of cystic duct remnants.
Observations of the present study also support those previous reports. Low insertion of cystic duct in the present case might have evaded surgeon’s attention during surgery which had resulted in the remnant duct. With dilation of the remnant duct a “neo-gall bladder” was formed which had resulted in the relapse of symptoms. As concluded by Shaw et al., (2004) MRCP was most useful and helped to diagnose the left out remnant duct after cholecytectomy in the present case. By presenting this interesting case about left out cystic duct after cholecytectomy and its involvement in post-operative complications, importance of knowledge about anatomy of extra-hepatic biliary apparatus is emphasized.
Acknowlegements: Sincere thanks to
i. Dean, Mahatma Gandhi Medical College & Research Institute
ii. Dr. Ananth Krishnan, Prof & HOD of Surgery, Mahatma Gandhi Medical College & Research Institute for guidance.with the formation of common bile duct stones?
Surg Endosc, 21: 48-52.
Suhocki PV, Meyers WC (1999) Injury to aberrant bile duct during cholecystectomy: a common cause of diagnosed error and treatment delay. Am J Roentgenol, 172: 955-959.
Marcos A (2000) Right lobe living donor liver transplantation – A review. Transplantation, 6:3-20.
Lamah M, Karanjia ND, Dickson HG (2001) Anatomic variations of extrahepatic biliary tree: review of world literature. Clin Anat, 14:167-172.
Fujikawa T, Takeda H, Matsuesue S, Nakamura Y, Nishimura S (1998) Anomalous duplicated cystic duct as a surgical hazard: A report of a case. Surgery Today, 28: 313-315.
Bernard P, Lettessier E, Denimal F, LeNeel JC (2001) Accessory cystic duct discovered by intra operative cholangiography during cholecystectomy. Amn Chir, 126: 1020-1022.
Hashimoto M, Hashimoto M, Ishikawa T, Lizuka T, Matsuda M, Watanbe C (2002) Right hepatic duct emptying into cystic duct – report of a case. Surg Endosc, 16: 359.
Loasnoff JE, Jones JW, Richman BW, Ranganekar NJ (2002) Hepato-cystic duct – a rare anomaly of the extrahepatic biliary system. Clin Anat,15; 314-315.
Singh I, Pal GP (2007) Chapter 14 In:
iii. Dr.Prakash, M.L., Prof & HOD of Radiology,
Human Embryology-8,edition. New Delhi:
Mahatma Gandhi Medical College & Research Institute for giving the awareness of Neo gall bladder & its importance.
iv. Dr.Sudha Rao, Prof & HOD of Anatomy, Mahatma Gandhi Medical College & Research Institute for encouraging me to document this rare case for the to disseminate this knowledge of variations
v. Dr. N.S. Kannan, Prof of Surgery & Controller of Examination, SBV University, Mahatma Gandhi Medical College & Research Institute for adding more reference to this case report
References
Taourel P, Bret PM, Renhold C, Barkun AN, Atri M (1996) Anatomic variation in biliary tree – diagnosis with MR Cholangio pancreatography. Radiology, 199: 521-527.
Turner MA, Fulcher AS (2001) The cystic duct normal anatomy and disease processes. Radiographics, 21: 3-22.
Tsitouridis I, Lazaraki G, Papastergion C, Pagalos E, Germanidis G (2007) Low conjunction of cystic duct with common bile duct does it correlate
Mac Millan India Limited. pp171-172.
Roggy M, Fugger A, Herbst R, Schulz F (1991) Reoperation after cholecystectomy: role of Cystic Duct Stump. HPB surg, 4:129-134.
Walsh RM, Ponsky JL, Dumot J (2002) Retained gall bladder /cystic duct remnant calculi as cause of post cholecystectomy pain. Surg Endosc, 16:981-984.
Tantia et al., (2008) Post cholecystectomy Syndrome: Role of Cystic duct stump – re intervention by laparoscopic surgery. J Minimum Access Surg,4: 71-75.
Wani NA, Khan NA, Shah AI, Khan AQ (2004) Post cholecystectomy Mirrizzi Syndrome: Magnetic Resonance Cholangiopancreatiography Demonstration.
Shaw CO, Hanlon DM, Fenlon HM, McEntee GP (2004) Cystic duct remnant and post cholecystectomy Syndrome. Hepato- Gastroenterology, 51: 36-38.