International Journal of Anatomical Sciences 2014, 5(2): 49-56
Research Article
Nicotine Exposure During Gestation on Neonatal Rat Testis Indicate Possibility of Fertility Impairment at Adulthood
Anitha V, Venkata Lakshmi N,* Sumathy G,‡ Karthik Ganesh M, Prakash S.
Department of Anatomy, Dr. Arcot Lakshmanasamy Mudaliar Postgraduate Institute of Basic Medical Sciences, University of Madras, Chennai, Tamil Nadu, India.
Department of Anatomy, Sathyabama University Dental College and Hospital, Chennai, Tamil Nadu, India.
Department of Anatomy, Sree Balaji Dental College and Hospital, Chennai, Tamil Nadu, India.
Key words: nicotine, gestation, teratogen, testis, infertility
Abstract: Nicotine is largely consumed as a component of cigarette during smoking. Nicotine exposure during pregnancy leads to many pregnancy related issues, developmental anomalies and increased possibility of adverse health conditions in the adulthood. Though nicotine use during pregnancy has been studied in human and same were co-related with number of adverse obstetrical and developmental outcomes. However, contributions from animal studies seem to be tremendous and also able to bring about the fact that nicotine alone may be a key chemical responsible for many adverse effects associated with maternal cigarette smoking on the progeny. This study was done using pregnant female Wistar Albino rats to investigate the effect of nicotine administration during individual trimesters and full gestation on testis of the neonates. The male pups were picked from the each litter and were used for this study. Observations showed gross change in testis with a decline in testicular size in full gestation treated group (Nic-Full-Trim) when compare to control, 1st (Nic-I-Trim) and 2nd (Nic-II-Trim) trimester treated rats. Histology of testis reveled seminiferous tubules with disorganized and degenerating cells in the lumen in nicotine administrate during 3rd trimester (Nic-III-Trim). In Nic-Full-Trim group the diameter of the seminiferous tubules and germ cell number were much reduced. The severity of the damage was more obvious in Nic-Full-Trim group which showed much reduced testicular size and tubules, degenerating cells and increased interstitial space with marked collagen deposition when compare to the rest of the nicotine treated groups. Increased Caspase-3 and NFκB expression in nicotine treated groups indicate activation of apoptotic pathway in germ cells. Observations indicate that Nic-III-Trim and Nic-Full-Trim group’s male progeny testis were severally affected by nicotine exposure and probably would show impaired fertility at adulthood.
Cigarette smoking which increases the risk of fatal diseases like cardiovascular diseases, coronary artery disease, myocardial infarctions, lung cancers, cerebrovascular incidents, etc. Nicotine is an addictive component of cigarettes and exists at high concentrations in the bloodstream of smokers (Benowitz, 1988). Stoppage of smoking during pregnancy can reduce damage to the developing fetus (Lindley et al., 2000; Pickett et al., 2003). Cigarette smoke is a complex mixture of toxic chemicals including nicotine, carbon monoxide, and several recognized carcinogens and mutagens. These toxicants are absorbed through the pulmonary vasculature and transported via the blood stream causing cytotoxicity, genotoxicity, and tumorigenicity throughout the body. Nicotine is metabolized primarily by the liver, and to a lesser extent, the lung and kidney, with the primary metabolite being cotinine (Stillman,.et al., 1986; Roger and Abbott, 2003).
Effects of Nicotine on Fetus
Pregnant women are exposed to various teratogens with or without their knowledge. With the modernization, most women are indulge in the habit of smoking and few are exposed to passive smoking at work place, public places etc. The follow-up investigations on these progeny indicate that they would develop infertility, diabetes, obesity, hypertension, neurobehavioral defects, and respiratory dysfunction. Cigarette smoking during pregnancy can lead to numerous obstetrical issues including, fetal growth restriction (Hammoud et al., 2005), placental abruption (Ananth et al., 1999), spontaneous abortion (George et al., 2006), sudden infant death syndrome (SIDS) (Mitchell and Milerad, 2006), placenta previa (Hung et al., 2007), preterm birth (Fantuzzi et al., 2007), stillbirth (Hogberg and Cnattingius, 2007) and low birth weight (Jaddoe et al., 2008).
From the experimental studies it is clearly evident that the active or passive exposure of pregnant women to nicotine toxicity causes adverse teratogenic effects on the various stages of embryonic develop-ment, leading to congenital anomalies. Nicotine (and its major metabolite cotinine) crosses the placental barrier and is found in fetal tissues in concentrations that are equal to, or greater than plasma nicotine levels in the mother (Dempsey and Benowitz, 2001; Ilett et al., 2003). In adult male cigarette smoking has also been associated with decreased sperm count, alteration in motility of the sperms, and overall increase in the number of abnormal sperms in humans (Kalikauskas et al., 1985) and decreases the level of testosterone (Sarasin et al., 2003).
The aim of the study was to analyze the deleterious effect of nicotine on testis of rats when exposed during embryonic period. This study was done using pregnant female Wistar Albino rats. Effect of nicotine administration during individual trimesters and full gestation on testis of the neonates, thereby delineate the vulnerable period for developing testis and to make out the germ cell loss in the early development periods. The male pups were picked from the each litter and were used for this study.
Materials and Methods
Animals Used
Female Wistar albino rats (Rattus norvegicus) used for this study. This species has very good adaptability, able to survive and breed under wide range of climatic conditions in variety of habitats. Albino rats have been extensively used as an experimental model for a variety of studies all over the world including embryological or developmental studies. With biological research point of view the rat and human share many similarities (Weihe, 1983).
Animal Maintenance
Details of the animal maintenance were given elsewhere (Suresh et al., 2009). The study was approved by the institutional ethical committee (IAEC no.01/004a/06). Animals were maintained according to the guidelines of the Canadian Council for Experimental Animal Care (1993) and the Committee for the Purpose of Control and Supervision of Experiments on Animals (CPCSEA), India (2003) guidelines for laboratory animal facility. Healthy female animals were randomly sorted into different five groups (vide infra). These rats were allowed to mate with a healthy proven fertile male rat. After confirming the pregnancy, these rats were subjected to nicotine hydrogen tartrate (Sigma-Aldrich, USA) administration at a daily dosage of 2 mg/kg of body weight (i.p.). Details of the animal grouping as follows,
- Group I – Control
- Group II – During 1st week of gestation i.e. 1 -7 days (Nic-I-Trim)
- Group III – During 2nd week of gestation i.e. 8 – 14 days (Nic-II-Trim)
- Group IV – During 3rd week of gestation i.e. 15 – 21 days (Nic-III-Trim)
- Group V – Full period of gestation i.e. for 21 days (Nic-Full-Trim)
Nicotine Administrated groups

The male pups from corresponding groups were selected from each litter. These pups were used for this study.
Histological Analysis
The testis were dissected out from the pups under over dose of anesthesia and fixed in Bouin’s fixative and 4% of para formaldehyde. Testes were subjected to gross measurements. The tissues were processed for paraffin sectioning and stained with haematoxylin & eosin and Masson’s trichrome (Collagen deposition). The stained section were observed under Nikon bright-field microscopic (Nikon Corporation, Japan) and immuno-histochemical staining to determine the extent of cellular damage through apoptosis using Caspase 3 and NFκb anti-bodies. Conventional stereological principles and accepted morphometric procedures as outlined by Elias and Hyde (1980), for morphometry in general was used in the present study to obtain quantitative information.
Results
Gross measurement of the testis showed decline in testicular size in all the nicotine treated groups (Plate 1).H & E staining: The testes from Nic-I-Trim and Nic-II-Trim groups showed degenerative changes in the seminiferous tubules.
In Nic-III-Trim group rat testis showed reduced seminiferous tubular diameter and decrease in germ cell number. The severity of the damage was more obvious in Nic-Full-Trim group rat testis with very much reduced tubular diameter and increased degenerating cells (Plate 2).
Plate 1: Morphology of testis taken from different experimental groups. Note the reduction in size of the testis taken from nicotine treated rats.
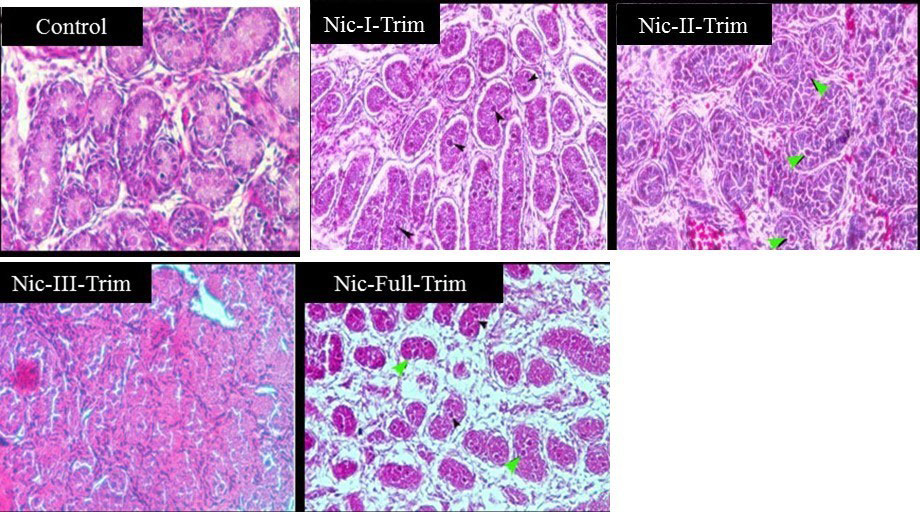
Plate 2: Photomicrograph of neonatal rat testis images from control and nicotine treated. Control pup testis showing normal histo-genesis of germ cells along seminiferous tubules.
Nicotine treated rat pup testis showed degenerative changes (black arrow head). Increased damages were observed in neonatal testis from maternal rat treated with nicotine for whole trimesters (Nic-Full-Trim group). Note few abnormal cells (giant cells) in the lumen of the tubules (green arrow). H & E 20x magnifications.
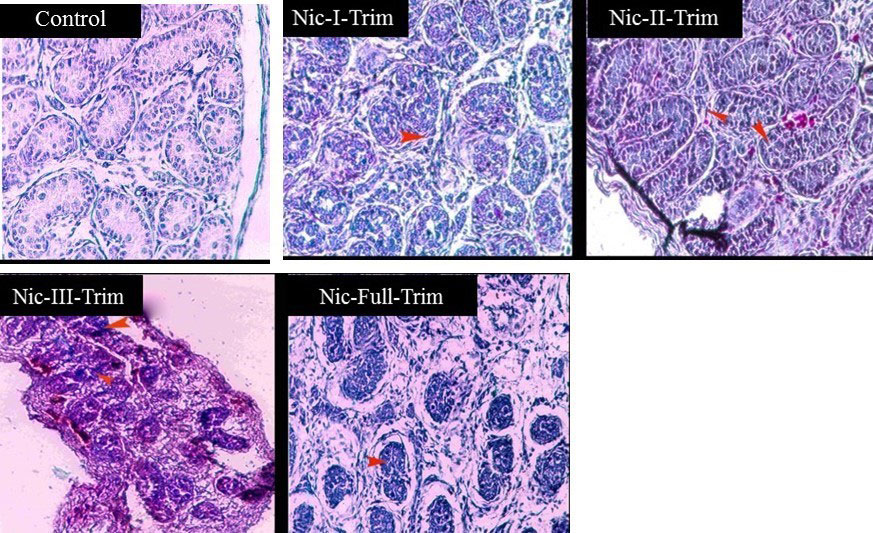
Plate 3: Photomicrograph of neonatal rat testis images from control and nicotine treated.
Increased collagen depositions were seen in nicotine treated rat pup testis (red arrow head) than the control. Collagen deposition was more pup’s testis which were treated with nicotine for whole trimesters (Nic-Full-Trim group). Masson’s trichrome staining 20x magnification.
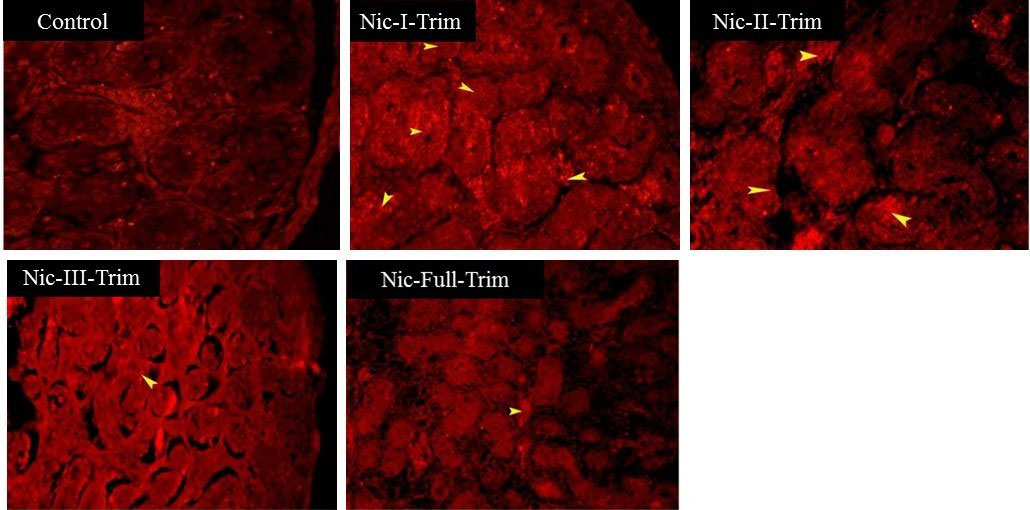
Plate: 4: Immuno-localization of Caspase 3 in neonatal testis
Image indicates increased or up-regulated Caspase 3 expression (arrow head) in the nicotine exposed pups testis when compare to control. Note expression was also merger in Nic-Full-Trim testis probably reduction in germ cells.
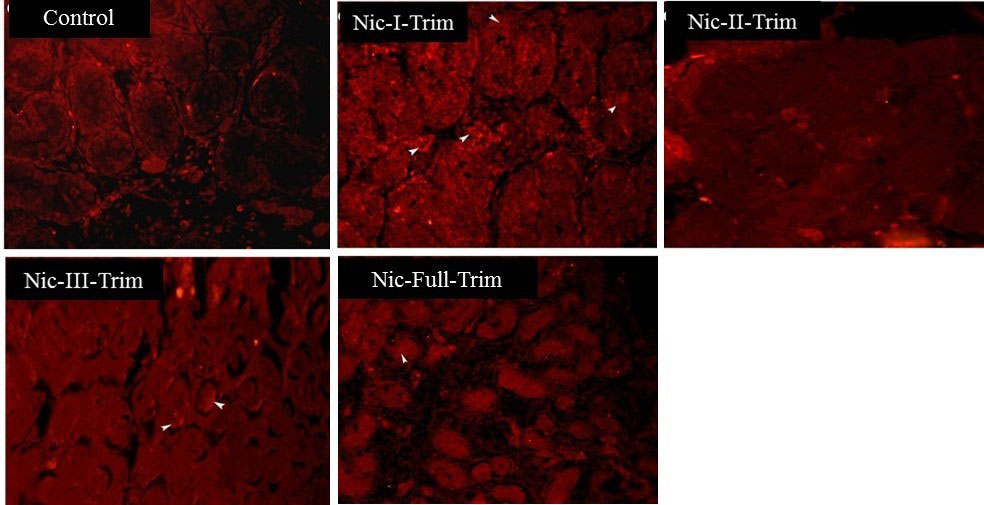
Plate 5: Immuno-localization of NFκB in neonatal testis.
Image indicates increased or up-regulated NFκB expression (arrow head) in the nicotine exposed pups testis when compare to control. Note expression was more in Nic-I-Trim testis than the Nic-Full-Trim, may be due to the impaired germ cell loss or proliferation.
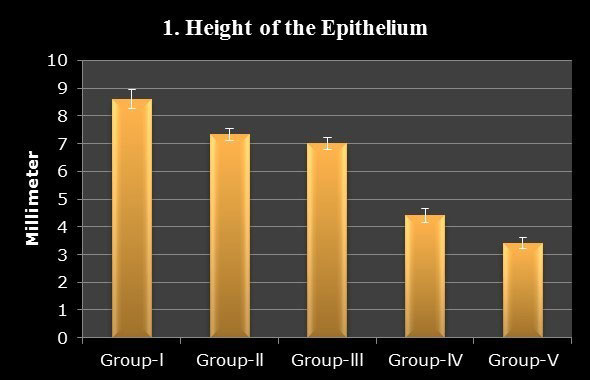
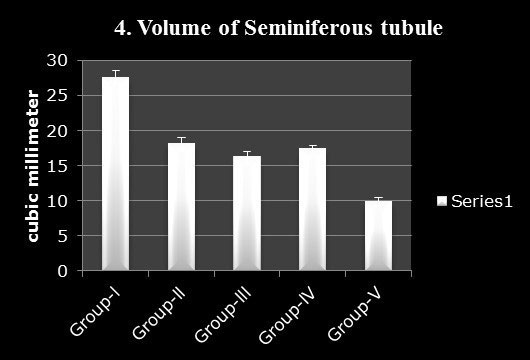
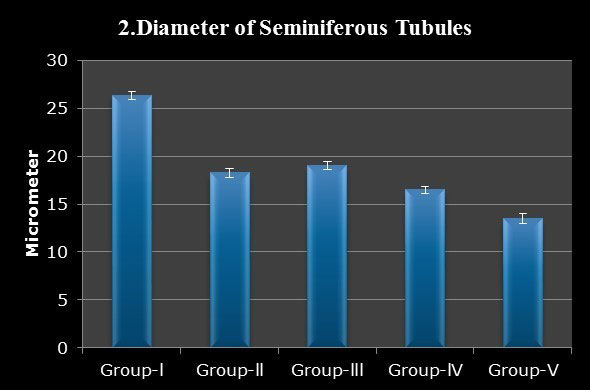
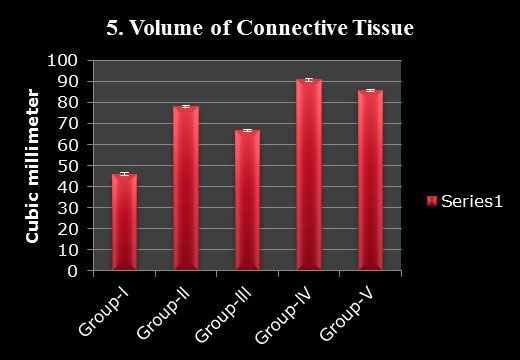
Masson’s Trichrome Staining:All the nicotine treated groups showed relatively increased collagen deposition when compare to control. However, collagen deposition was markedly increased in Nic-Full-Trim group rat testis indicating atrophic changes and cellular depletion (Plate 3). Caspase 3 and NFκb anti-body staining indicate apoptotic changes in Nic-III-Trim and Nic-Full-Trim rat testes (Plate 4 & 5) Histomorphometry: Histo-morphometrical analysis of testis showed decrease in the height of the germinal epithelium, diameter of the seminiferous tubules, volume of the seminiferous tubules, and volume of the epithelium whereas, the connective tissue volume proportion was increased in nicotine treated rat testis (Graph 1-5).
Discussion
Smoking is a major health hazard. The adverse effects of prenatal cigarette smoke exposure on human reproductive outcomes are a major scientific and public health concern. The human related scientific literature about the long-term effects of nicotine use during pregnancy is lacking, but there is substantial evidence from animal studies showing that fetal and neonatal nicotine exposure leads to widespread adverse postnatal health consequences. In our study maternal nicotine exposure during gestation caused defective gonad development which may lead to delayed puberty and reduced fertility in later life.
Developmental exposure to cigarette smoke is associated with numerous negative reproductive outcomes, ranging from alterations in germ cell morphology to an increased morbidity and mortality of offspring (DiFranza and Lew, 1995).
Histological observation from the present study revealed distorted seminiferous tubular wall and cellular degenerative chan-ges in 1st and 2nd weeks of nicotine treatment. In 3rd week of gestation (Nic-III-Trim) showed reduced tubular size and reduced germ cells population which was also supported by histo-morphometric observa-tions. Indeed, nicotine administration or exposure to cigarette smoke inhalation to rats and hamsters results in testicular degeneration (Viczian, 1968). In full term nicotine treated testis (Nic-Full-Trim) showed reduced testicular size and increased germ cell degeneration, degenera-ting cells in the tubules, increased interstitial space etc. Apart from these factors, the possible explanation for the pathological changes may be due to direct effect of nicotine on the fetus by its metabolite cotine, which can inhibit rat testis androgen biosynthesis (Fowler et al., 2008).There are evidences stating that nicotine freely crosses the placenta and has been found in the amniotic fluid and umbilical cord of neonates (Luck et al., 1985). Intrauterine exposure to nicotine also results in decreases in birth weight (Tizabi et al., 2000) indicating poor transportation of nutrients from maternal to developing fetus which could affect the general organ growth in late trimesters.
This was obvious testicular weight Nic-III-Tim and Nic-Full-Trim. Collagen deposition was markedly increased in Nic-Full-Trim group rat testis. The collagen was deposited in the interstitial space as a result of tubular atrophy and in the lumen as a result of cellular depletion.
The germ cell degeneration by nicotine treatment may be because of the low intra-testicular concentrations of testosterone, as high level of testosterone in testis is essential for the normal spermatogenesis as well as for the maintenance of the structural morphology and the normal physiology of seminiferous tubule (Sharpe et al., 1992). The testosterone is required for the attachment of different generations of germ cells in seminiferous tubules, and therefore, the low level of intra testicular testosterone may lead to the detachment of germ cells from the seminiferous epithelium and may initiate germ cell death (Blanco-Rodriguez and Martinez-Garcia, 1988). Besides, nicotine and its metabolite cotinine easily enter into the blood circulation of testis and can have a direct cytotoxic effect by damaging DNA (Sepaniak et al., 2006).
Programmed cell death, also known as apoptosis, is required for normal spermatogenesis in mammals and is believed to ensure cellular homeostasis and maintain the fine balance between germ cells and Sertoli cells. The proper regulation of the caspase cascade plays an important role in sperm differentiation and testicular maturity. However, caspases have been implicated in the pathogenesis of multiple andrological pathologies such as impaired spermato genesis, decreased sperm motility, increased levels of sperm DNA fragmentation and in toxicity. Increased Caspase-3 and NFκB expression in nicotine treated groups indicate activation of apoptotic pathway in germ cells. Nicotine and its metabolite cotine might have caused toxicity and initiated the apoptotic pathway, which is evidenced by increased activity of Caspase-3 and NfkB activity.
Thus indicate that Nic-III-Trim and Nic-Full-Trim group’s male progeny testis were severally affected by nicotine exposure and probably would show impaired fertility at adulthood. Findings show that intra-uterine tobacco smoke increased the risk of oligozoospermia in offspring.
References
Ananth CV, Smulian JC, Vintzileos AM (1999) Incidence of placental abruption in relation to cigarette smoking and hypertensive disorders during pregnancy: a meta-analysis of observational studies. Obstet. Gynecol,, 93: 622–628.
Benowitz NL, Porchet H, Sheiner L, Jacob P (1988) Nicotine absorption and cardiovascular effects with smokeless tobacco use: Comparison with cigarettes and nicotine gum.Clinic Pharmacol Therapeut,,44: 23–28
Blanco-Rodriguez J, Martinez-Garcia C (1988) Apoptosis precedes detachment of germ cells from the seminiferous epithelium after hormonal suppression by short-term oestradiol treatment of rats.Int J Androl,21: 109–115.
Committee for the Purpose of Control and Supervision on Experiments on Animals (CPCSEA) guidelines for laboratory animal facility. Committee for the Purpose of Control and Supervision on Experiments on Animals (2003). Ind J Pharmacol 335:257–74.
Dempsey DA, Benowitz NL (2001) Risks and benefits of nicotine to aid smoking cessation in pregnancy.Drug Saf, 24: 277-322.
DiFranza JR, Lew RA (1995) Effect of maternal cigarette smoking on pregnancy complications and sudden infant death syndrome.J Fam Pract,40: 385-94.
Elias H, Hyde H (1980) An elementary introduction to stereology.Am J Anat, 159: 411 – 446.
Fantuzzi G, Aggazzotti G, Righi E, Facchinetti F, Bertucci E, Kanitz S, et al. (2007). Preterm delivery and exposure to active and passive smoking during pregnancy: a case-control study from Italy.Paediatr.Perinat. Epidemiol,21: 194–200.
Fowler PA, Bhattacharya S, Gromoll J, Monterio A, O’Shaughnessy PJ (2009) Maternal Smoking and Developmental Changes in Luteinizing Hormone (LH) and the LH Receptor in the Fetal Testis.J Clinic Endocrinol Metab,94: 4688-4695
George L, Granath F, Johansson AL, Anneren G, Cnattingius S (2006). Environmental tobacco smoke and risk of spontaneous abortion.Epidemiology,17: 500–505.
Hammoud AO, Bujold E, Sorokin Y, Schild C, Krapp M, Baumann P (2005). Smoking in pregnancy revisited: Findings from a large population-based study. Am J Obstet Gynecol,192: 1856– 1862
Hogberg L, Cnattingius S (2007). The influence of maternal smoking habits on the risk of subsequent stillbirth: is there a causal relation?BJOG, 114: 699–704.
Hung TH, Hsieh CC, Hsu JJ, Chiu TH, Lo L M, Hsieh TT (2007). Risk factors for placenta previa in an Asian population.Int. J. Gynaecol. Obstet,97: 26–30.
Jaddoe VW, Troe EJ, Hofman A, Mackenbach JP, Moll HA, Steegers EA, Witteman JC (2008). Active and passive maternal smoking during pregnancy and the risks of low birthweight and preterm birth: the Generation R Study.Paediatr. Perinat. Epidemiol,22:162–171.
Kulikauskas V, Blaustein D, Ablin RJ (1985) Cigarette smoking and its possible effects on sperm.Fertil Steril,44: 526-8.
Lindley AA, Becker S, Gray RH, Herman AA (2000). Effect of continuing or stopping smoking during pregnancy on infant birth weight, crown-heel length, head circumference, ponderal index, and brain:body weight ratio. Am J Epidemiol,152: 219–225.
Luck W, Nau H (1985). Nicotine and cotinine concentrations in serum and urine of infants exposed via passive smoking or milk from smoking mothers. J Pediatr,107: 816–820.
Mitchell EA, Milerad J (2006). Smoking and the sudden infant death syndrome. Rev. Environ. Health,21: 81–103.
Olfert ED, Cross BM, McWilliam AA. Guide to the care and use of experimental animals. Volume 1. 2nd ed. Canadian Council for Animal Care; 1993.
Pickett KE, Wakschlag LS, Dai L, Leventhal BL (2003). Fluctuations of maternal smoking during pregnancy.Obstet. Gynecol,101: 140–147.
Rogers JM, Abbott BD (2003) Screening for Developmental Toxicity of Tobacco Smoke Constituents.Toxicol Sci,75: 227-228.
Sarasin FP, Hanusa BH, Perneger T, Louis-Simonet M, Rajeswaran A, Kapoor WN (2003) A Risk Score to Predict Arrhythmias in Patients with Unexplained Syncope.Acad Emerg Med,10: 1312–1317.
Sepaniak S, Forges T, Gerard H, Foliguet B, Bene MC, Monnier- Barbarino P (2006) The influence of cigarette smoking on human sperm quality and DNA fragmentation.Toxicology,223: 54–60.
Sharpe RM, Franks S (2002). Environment, lifestyle and infertility—an inter-generational issue.Nat. Cell Biol,4: 33–40.
Stillman RJ, Rosenberg MJ, Sachs BP (1986). Smoking and reproduction. Fertil. Steril,46: 545–566.
Suresh S, Prithiviraj E, Prakash S (2009) Dose- and time-dependent effects of ethanolic extract of Mucuna pruriens Linn. seed on sexual behaviour of normal male rats.J Ethnopharmacol,22:497–501.
Tizabi Y, Perry DC (2000) Prenatal nicotine exposure is associated with an increase in [125I] epibatidine binding in discrete cortical regions in rats. Pharmacol Biochem Behav, 67:319-23.
Viczián M (1968) Experiences with sperm examination of smokers. Orv Hetil,19: 1077-9.
Weihe WH (1983) The UFAW handbook on the care and management of laboratory animals : The Laboratory rat, 309-30
